Macular Degeneration

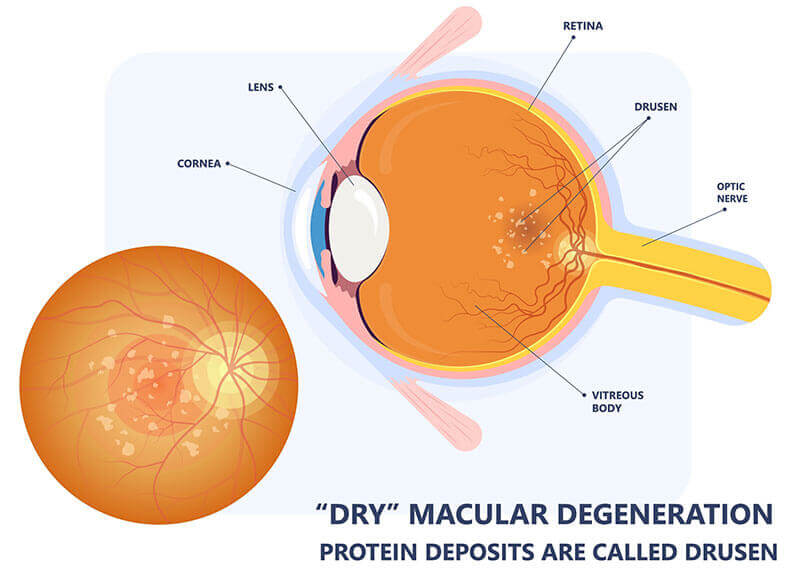
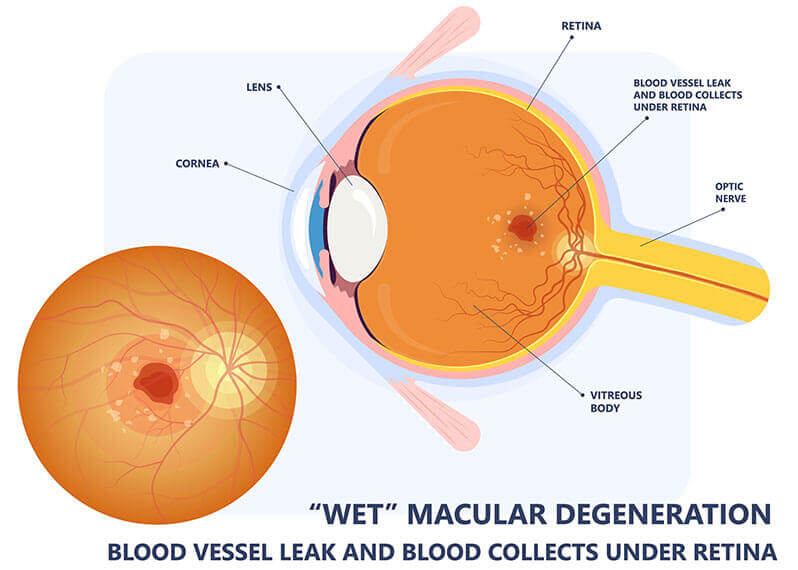
There are two types of Age-Related Macular Degeneration: Dry AMD and Wet AMD. Both forms of ARMD affect only your central vision, the part of your eyesight used to recognize faces, read, drive, and see fine detail. For simplicity, this is the middle focus spot in your vision that you refer to as clear or blurry, and the part of the retina affected is called the macula, hence the disease is named macular degeneration. It can affect one or both eyes but does not affect your peripheral vision or side vision.
The Dry type is more common occurring in up to 90% of cases and is fortunately more benign since it is slowly progressive over a period of many years. Although it may start as early as age 52, it rarely causes severe vision loss until age 75 and above, typically affecting light colored eyes and people with fair skin, high blood pressure, or a history of smoking. It is important to diagnose early because vitamins can help slow the progression and limit the chances it turns into the wet type. In Dry AMD, proteins called drusen form little yellow clumps and bumps under the tissue causing distortion, difficulty reading, changes in color perception, and darkened central vision. In severe cases, thinning of the receptor cells occurs similar to hair loss in balding.
The Wet type affects 10% of AMD patients and refers to abnormal blood vessels growing under the retina similar to weeds in a garden. The good news is that there are excellent treatments which can improve recent vision loss in up to 36% of patients and with continued ongoing treatment can stabilize and prevent further vision loss. It is exceptionally important to have this diagnosed immediately upon the initial symptoms to achieve the best visual result possible. Once the blood forms a scab and hardens, then there is nothing further that can be done to restore or improve vision. Although you may become legally blind in one or both eyes, you will not be totally blind from macular degeneration.
If you or someone you know are having any of these symptoms, especially if they are within the past few days or 1-2 weeks, click here to schedule an immediate appointment.
There are several types of diagnostic testing that can be performed in addition to a dilated eye exam where an eye physician will look into the back of the eye and examine the retina, macula, and optic nerve. OCT testing is a noninvasive photo of the layers of the retina comparing elevations, thicknesses, and atrophy of the retinal layers to give an indication as to the structural health of the macula, whereas a fundus photo is a picture of the back of the eye which can show exactly what your eye physician sees when examining your eye. Fluorescein Angiography is a test in which vegetable dye is injected into a vein and wherever there is a break in a blood vessel in the back of the eye a puddle will form in the photo, pinpointing the location and severity of the disease. This helps the retinal specialist determine which treatment will work best for you.
Diabetic Retinopathy

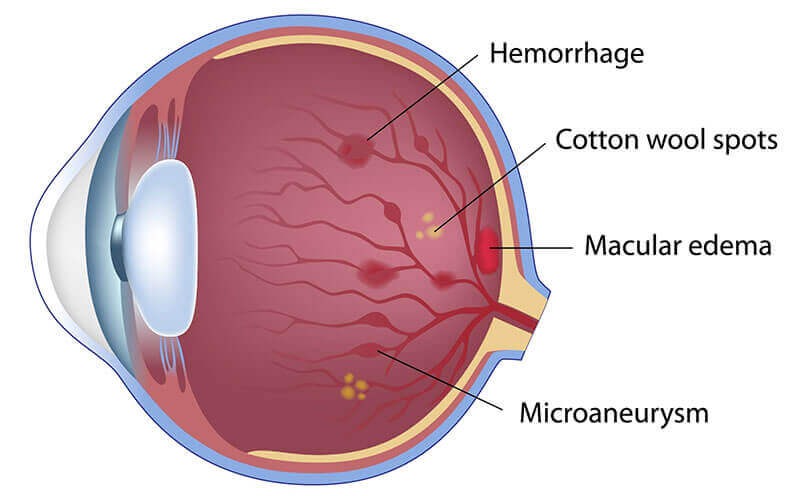
Diabetic Retinopathy is a complication of diabetes in which elevated blood sugar levels damage retinal blood vessels similar to a metal pipe that rusts until holes form in the tube that causes fluid, blood and fat to leak into the retinal tissue damaging your camera film. It can occur in both type 1 and type 2 diabetics, and high blood pressure, elevated cholesterol, and smoking make it worse. It can also occur in pregnant women who have gestational diabetes. Diabetic retinopathy can increase your chances of developing other serious eye conditions, including glaucoma, cataracts, retinal detachment , and blindness. It is the most common cause of vision loss in diabetics.
Stages of Diabetic Retinopathy
Non-Proliferative Diabetic Retinopathy (NPDR) is categorized as mild, moderate or severe, depending upon how long you have had diabetes and how well your blood sugar is managed. It typically takes five years to develop diabetic retinopathy from the time of diagnosis, but since no one knows the exact time of onset of diabetes, it is important to have a baseline exam once the diagnosis has been made by your primary care doctor. Fluctuating vision related to changes in your blood sugar is one of the early signs of diabetes and occurs before retinopathy shows up.
Moderate NPDR is often associated with fluid build up in the macula referred to as diabetic macular edema which can affect your ability to see fine detail, read, drive and more.
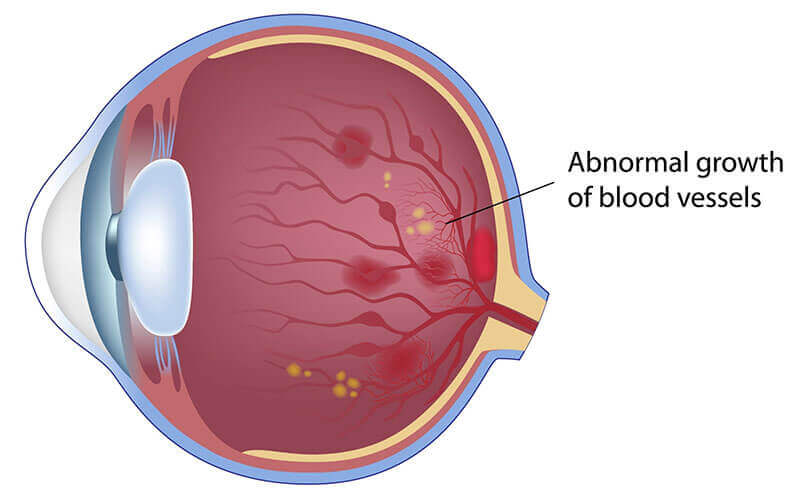
Severe NPDR occurs when blood vessels become increasingly blocked which cuts the retina off from its blood supply. Scar tissue begins to form and the retina starts to generate new blood vessels which are increasingly leaky and fragile. At this stage, patients may experience vision problems like blurriness and dark spots.
Proliferative Diabetic Retinopathy (PDR) is the most advanced stage and occurs when abnormal blood vessels grow into the retina and vitreous fluid and cause scar tissue to form. In severe cases, the scar tissue will pull the retina out of position causing a tractional retinal detachment. This advanced stage can lead to permanent vision loss.
Non-Proliferative Retinopathy
Proliferative Retinopathy
Diabetic Retinopathy Symptoms
In the early stages of diabetic retinopathy, many patients experience no symptoms or problems with vision. It’s not until the later stages that symptoms typically begin to appear. These symptoms include blurry vision, eye floaters, loss of central vision, black spots in vision, and inability to see color.
Diagnosis is made by
Dilating the eye and performing ophthalmoscopy whereby a specialist examines the back of the eye. Fluorescein Angiography, Fundus Photos, and OCT can be used to document the extent of leaking blood vessels as well as determine the source of leaks, lack of blood flow and extent of swelling and damage to the retina.
Treatment
Eye injections: Medications can be used to reduce swelling and inhibit the growth of abnormal blood vessels in the eye.
Focal laser treatment: Light energy is delivered to the back of the eye to cauterize leaking blood vessels.
Vitrectomy: An outpatient surgical procedure used to repair retinal detachments can also be used to remove the gel or scaffolding from the eye that enables the abnormal blood vessels to grow. In addition, scar tissue can be removed at the same time.
Retinal Vein Occlusions and Artery Occlusions
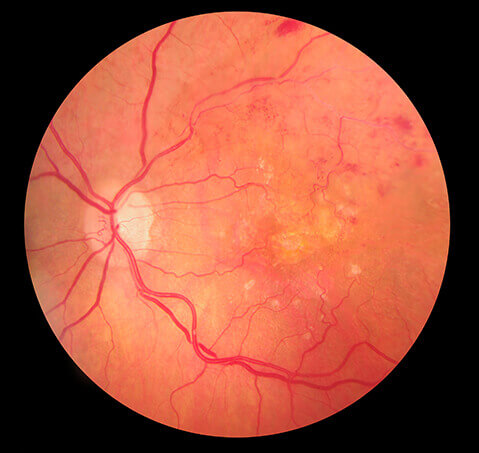
The retina is the camera film in the back of the eye that enables us to see and just like any other tissue or organ, it needs proper blood flow to function properly. The retinal vasculature is a system that consists of arteries, veins, and their branches, much like a tree or a leaf. The larger vessels are central and the smaller ones are referred to as branches. If the central retinal artery becomes blocked from plaque, all vision can be lost permanently, as this would be an “eye stroke”.. If it involves a branch of the artery, then a pie shaped portion of the vision will be lost. In the event of a vein occlusion, they also can be either central or peripheral. Vein occlusions occur because the artery usually compresses the vein which results in congestion in the eye so that there is fluid leakage and stagnant blood flow. Unlike arterial occlusions, vein occlusions respond to treatment. However, with an arterial occlusion, it is one of the few instances where your eye doctor can save your life.
The causes of these conditions are high blood pressure, diabetes, obesity, high cholesterol, smoking, cardiovascular disease, age, blood clotting disorders, hardening arteries, and inflammatory conditions.
Diagnosis is made by
Dilating the eye and performing ophthalmoscopy whereby a specialist examines the back of the eye. Fluorescein Angiography, Fundus Photos, and OCT can be used to document the extent of leaking blood vessels as well as to determine the source of leaks, lack of blood flow and extent of damage and swelling to the retina.
Treatment
Retinal vein and artery occlusions are generally treated by managing the underlying causative factors such as cessation of smoking, better management of blood pressure and cholesterol, sugar control in diabetes, and weight loss. Medications may also be injected into the eye to stop abnormal blood vessels from leaking in vein occlusions. Laser treatment can also cauterize leaking blood vessels.
Flashes, Floaters, Retinal Tears and Detachments

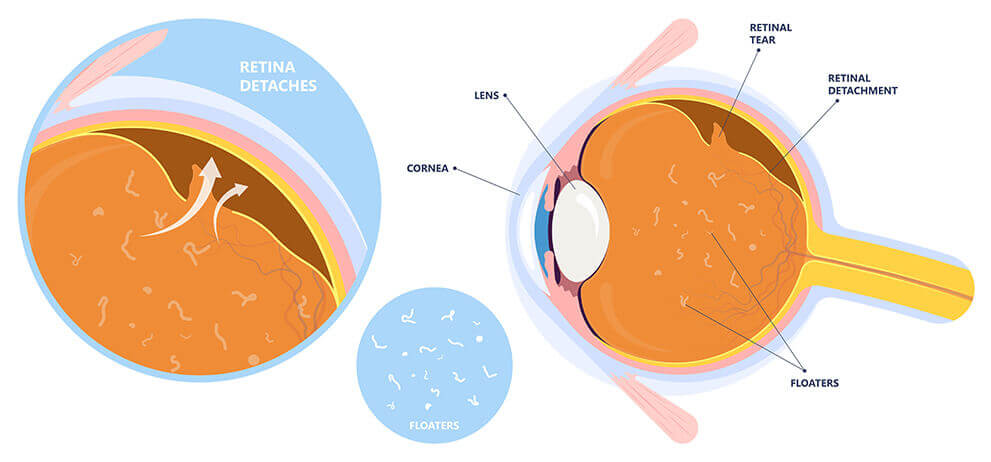
The retina is the thin layer of light sensitive tissue that covers the inner wall of the back of the eye and because it is delicate in structure, it is susceptible to defects such as retinal tears. This can cause a sudden onset of flashes and floaters in your vision, which can look like dark spots, squiggles, or hairs. If left untreated, retinal tears can lead to retinal detachment, which is when the retina separates from the back of the eye. Retinal detachments are a medical emergency that can cause complete vision loss in the affected eye.
Because it is always easier to treat a retinal tear compared to a retinal detachment, not to mention the improved outcomes in terms of shortened length of recovery and final visual result, it is important to address the warning signs of a retinal tear. Flashes typically look like little strands of light flickering across your visual field. For some patients, flashes may appear as a streak of light, a bright spot, a jagged line of lightning, a firework-like burst of light, or a camera flash. Floaters typically look like small floating shapes across your visual field. Some patients describe these shapes as being similar to spots, squiggly lines, small shadows, and thread-like strands. In terms of color and opacity, they can be translucent or dark. You may also experience a layer of darkness over your vision or blurriness. These symptoms may appear suddenly and intensify right before a retinal detachment occurs.
If you or someone you know is experiencing these symptoms within the past 1-3 weeks, please click here to schedule a prompt evaluation.
Treatment of Retinal Tears
Your retina specialist will place a lens on the front of the eye and shine a beam of light onto the retinal surface which will cauterize the tissue and create healthy scar tissue so that fluid cannot get under the retina and cause a blister to form which is then a retinal detachment.
Treatment of Retinal Detachment
This requires a trip to the operating room where your retinal specialist will remove all of the clear fluid from within the eye and remove the fluid from under the retina, then apply laser treatment to seal the tear and hold the retina in position using a gas or oil bubble. For inferior retinal detachments, a scleral buckle or “rubber band” may be placed around the outside of the eye.
Macular Conditions
The macula is a round pigmented area measuring 5.5 mm in diameter which is responsible for central vision, that is, the ability to read, see fine details, and see color. It is very delicate because it is extremely thin and is comprised of cones making it susceptible to a wide range of conditions, the most well known being age-related macular degeneration, which is deterioration of the macula from aging. When the macula becomes damaged, it can cause several issues with the most serious being loss of central vision.
Macular Hole
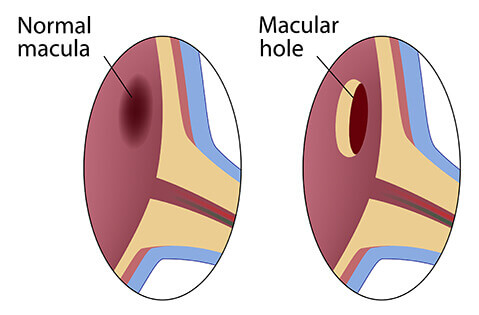
A macular hole is a break or separation in the macula. Typically an after effect of a posterior vitreous detachment or aging process whereby the vitreous fluid separates from the retina, this separation can sometimes pull on the macula forming a hole. The key to a macular hole formation is the horizontal separation of the macula caused by traction. Macular holes can be repaired through surgery by relieving this traction or sideways tension. Typically, better results are achieved when the hole is recent.
Macular Edema
Macular edema is when fluid leaks into the retina resulting in swelling caused by abnormal or damaged blood vessels in the eye. Conditions which cause macular edema are:
- Diabetes
- Retinal vein occlusion
- Macular degeneration
- Inflammatory eye diseases
- Eye injuries
- Hereditary retinal diseases such as retinoschisis or retinitis pigmentosa
- Vitreomacular Traction Syndrome
- VMT is a complication of a posterior vitreous detachment in which case the traction is vertical and lifts the tissue upward as opposed to sideways as in epiretinal membranes and macular holes.
Common Symptoms of Macular Conditions
- Difficulties with central vision
- Blurring or distortion
- Difficulty reading or seeing fine detail
- Floaters
- Gray area in center of vision
- Changes in color vision
How Macular Conditions Are Diagnosed
Eye dilation: The eyes are dilated using drops so the physician can look inside your eye at the retina.
Ophthalmoscopy: a light is shined into the eye so your doctor can determine if there is any damage or conditions in the macula region.
OCT: a “seeing” laser captures cross-sectional images of the retina, macula, and/or nerve. It is used to determine the presence of fluid or damage to the macula.
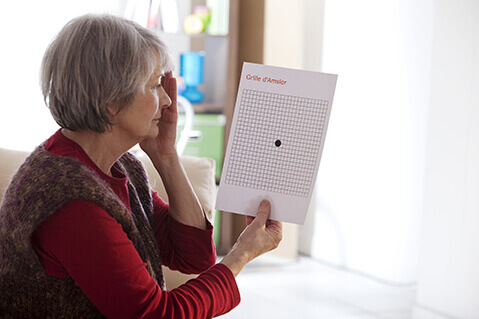
Ambler Grid: a dot in the center of graph paper can tell whether there is a defect in the patients vision.
Ultrasound: non-invasive imaging used to identify structural retinal issues.
Fluorescein angiography: a dye test used to show leakage of blood vessels within or under the retina.
Macular Conditions Treatment
There are several ways to treat or manage macular conditions. The more common methods include:
Managing underlying conditions and risk factors: Some macular conditions such as macular puckers are not treated at all beyond monitoring the condition and managing any underlying conditions or risk factors. Some of the most important risk factors to keep in mind are diabetes, high blood pressure, high cholesterol, smoking, aging, and cataract surgery.
Medications: Anti-vascular endothelial growth factor injections help to prevent abnormal blood vessel growth in the eyes. Avastin, Lucentis, and Eylea are commonly used to treat wet macular degeneration, diabetes, and vein occlusion. Macular edema is commonly treated with steroid injections.
Focal laser therapy or photocoagulation: This procedure uses a high-energy laser beam to seal abnormal blood vessels so that they stop bleeding, decreasing further damage to the macula.
Vitrectomy: A surgical procedure used to remove the vitreous fluid inside the eye so the macular can be repaired by removing scar tissue in macular puckers, macular hole, and vitreomacular conditions.
Epiretinal Membrane / Macular Pucker
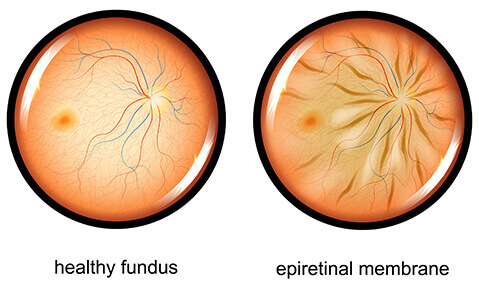
An epiretinal membrane, also known as a macular pucker, occurs when scar tissue forms on the surface of the macula or center of the retina. The scar tissue usually develops because as the fluid in the eye ages, it tends to harden in this area and forms a sheet of cells, much like an egg that gets cooked turns from a liquid to a solid. This scar tissue can be peeled very gently from the surface of the retina if it impacts your vision significantly. The good news is that this procedure is elective and does not require surgery unless the vision is 20/40 or worse. If you also have a cataract, simple cataract surgery may be all that is needed to get your vision to where you want it to be.
A macular hole is a more advanced form of an epiretinal membrane where the scar tissue pulls on the very thin fovea or center of the macula to cause a small hole to form, hence the term macular hole. The center of the vision will tend to be distorted with a dead spot where two or more letters in a word won’t appear. Results of a macular hole repair are best if surgery occurs within several weeks of symptom development. A vitrectomy with removal of all fluid in the back of the eye plus gentle removal of the scar tissue and gas bubble placement often results in 90% closure rate with one operation.
